Dealing with an eating disorder’s double dose of stigma – from public and self
Dealing with an eating disorder’s double dose of stigma – from public and self
by June Alexander
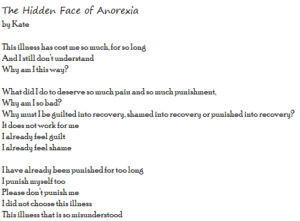
Engaging in the world beyond an eating disorder is scary because it means facing up to a double whammy of stigma driven a.) by the public and b.) from within. This post, drawn from Using Writing as a Therapy for Eating Disorders—The Diary Healer, digs through the layers to expose this serious issue.
The task is complex. Michael Levine explains why:
“One of the seductive traps and suffocating torments of an eating disorder is born of the sense that one can survive—indeed must survive and thrive—in private, within the confines of one’s own mind, with its personal rules, personal anxieties, personal convictions, and personal shame. This turning inward is reinforced and strengthened by many phenomena, including trauma, loss of control, self-deception, self-loathing, other people’s anger and rejection, and eventually stigma. And, of course, once again, painful self-consciousness is also strengthened by the eating disorder’s constant reminder of your rules for salvation, your failure to live up to them, and your opportunity to escape this emotional hothouse by mindless habit and/or rigid action, the price of which is more shortcomings, guilt, shame, and self-disparagement.”
– From the foreword to Using Writing as a Therapy for Eating Disorders—The Diary Healer
So what is stigma?
Stigma is stereotype, prejudice, and discrimination. Public and self-stigma hamper the lives of many people with eating disorders and other forms of mental illness. Professor Patrick Corrigan, in the preface to Coming Out Proud (2015), describes the two types of stigma:
“Public stigma occurs when the population endorses stereotypes about mental illness (people are dangerous, incompetent, and responsible for their mental illness) and discriminates as a result. Many of the employment, independent living, and health goals of people with mental illness are blocked by a public that endorses prejudice.
Self-stigma occurs when some people internalize the stereotypes of mental illness, applying it to themselves. Self-stigma harms peoples’ sense of self- esteem and self-efficacy leading to the “why try” effect. (Why should I try to get a job, study, live on my own, recover….). For someone already depressed and anxious, or has an eating disorder, self-stigma deepens the sense of shame that accompanies their illness.”
To be stigmatized is literally to be given a mark or brand that signals disgrace and, at best, second-class status in a society. In many so-called modern and developed societies the label of “mental illness” is stigmatizing because it is viewed as a euphemism for “crazy,” “wacko” or “truly weird.”
Often even the ostensibly humane label “mentally ill” carries stereotypical beliefs and negative emotional reactions (for example, fear, disgust, pity, and opportunist exploitation) that revolve around being childish and immature, weak, irresponsible, unworthy of inclusion, dangerous or out of control.
The double challenge
The perception of others, when accompanied by self-acceptance of the stigma and its stereotypes, can hamper healing. Derogatory labels from others peppered my diaries. I noted them as if to confirm and affirm the equally derogatory labels of my own. Together they demeaned and shot holes in my identity, and strengthened my illness.
At vulnerable times, in family, relationship and work environments, I felt I deserved all critical name-calling, and often my behavior reflected this. When told “you are the problem” often enough, it is easy to start believing it, and become “the problem,” imprisoning you more within the eating disorder and isolating you further from self.
Doctors had to work hard to convince me that I was not neurotic and that I was genuinely, sane and worthwhile. Therefore, in many ways, recovery had to include re-storying of perceptions as both participant and observer of self. I had to feel and see myself in a more positive way.
Suggestions that an eating disorder is a personal weakness can contribute to a rapid build-up of shame, alienation, and hopelessness. The effect is especially damaging when occurring in the very places you expect to feel safe and unjudged, like in your home and healthcare environment. Maddy explains how easily it can happen:
“I was getting out of bed for my six o’clock dinner, and a female nurse came in to supervise. She looked and said, ‘You don’t look that thin, I mean, you are short, so for your height you don’t look that thin and don’t look anorexic.’ I was too scared to tell her how hurt I felt because I am always worrying about if people like me. Afterwards, I wanted to just run away, but was too worried about disappointing my family.”
– Maddy
Let’s tell our stories
Associate Professor, Paul Rhodes, encourages story-telling to help address the stigma:
“We need to recognize we all created this stigma; it is a social phenomenon, a product of our superficial, performance-oriented culture, our collective unease with affect, our disconnection from self. The best way to overcome it is through hearing people’s stories.”
Reading narratives of how others have coped with mental health challenges, and embodying their insights into your own life story, can help to dismantle and eventually reject unhelpful ways of thinking. The process, the “doing,” of writing a diary and reading stories about developing, living with, and maintaining a sense of self separate from the illness can assist the gradual but essential shift in the social construction, and re-storying of harmful beliefs.
Stereotypes and fallacies
Beyond the perception of self and close others, wider powerful cultural beliefs and practices can reinforce misguided notions that “thin is good” and another stereotype, “fat is bad.” Such “in your face” inferences can hinder recovery from an eating disorder. Another cultural misconception is that only young people have eating disorders. Adults suffer, too—often since childhood and often in silence, feeling too ashamed to share their secret and seek help (see, e.g., Maine et al., 2015).
Jenny, 38, until she heard my story, thought she was the only adult with an eating disorder. Her greatest sadness was that the passage of years had led some family members to misunderstand her illness behaviors, at times alienating her from their life.
Equally, if not more damaging, are misconceptions in the health services environment. During a relapse requiring inpatient care, Jenny overheard a nurse, standing outside her room in the corridor, say to another nurse: “You would think she would be over this by now, wouldn’t you.”
Community-based prejudice and misconception
Besides the illness itself, stereotypes around race, gender, color, culture, ethnicity, immigrant populations and class may preclude you from feeling like you belong, and lead to stigmatization. In this way, community-based prejudice and misconception aggravates the isolating aspects of an eating disorder. Even being educated and “good-looking” can add to your problems. I was told: “You are intelligent, you have a lot going for you, surely you can see this is holding you back? Why are you being weak in this one area?”
Doctors and friends considered Andrea, a diligent and bright student, “too smart” to have an eating disorder. They could not seem to understand that, as with the onset of any serious illness, logic had no role in the development of her eating disorder, or in continuing to elaborate and carry out its cognitive, emotional, and behavioral demands. It is true Andrea did place ultimately destructive expectations on herself, but even her high level of intelligence and scientific problem-solving ability did not enable her to understand either how she “knew” what she needed to do to recover or why she was unable to put those healing behaviors into practice.
She stepped out of the resulting harsh self-judgments and intense frustration by writing about her irrational thoughts and behaviors and, paradoxically, finding logic and hope in the irrational. For example, Andrea began to understand what purposes her eating disorder was serving in her life.
“You don’t look like you have an ED”
Bingeing and purging caused Angel to feel “incredible” shame. She also felt stigmatized— branded or stained with disgrace—because she could not control, let alone stop, the cycle. The result was an unhealthy compromise with herself and others: Angel was often comfortable talking with health professionals and friends about her anorexia nervosa, but became secretive about more bulimic-type behaviors. She looked “normal” and felt expectation to behave so; the pressure was great. During this difficult phase, Angel’s diaries became a trusted place to troubleshoot an instance where she had binged and purged and to make a written commitment not to do it again.
Making such disclosures in her diary helped Angel get the problem outside her mind, and the resulting distance and perspective helped her to feel more hopeful while easing humiliation and guilt. Other times the process of describing the situation in her diary enabled her to locate, identify and analyze the emotion behind triggers, then commit to attending to the emotion as a way of minimizing or avoiding those triggers. “This approach,” Angel explains, “allowed me to feel okay about having binged/purged, and hopeful that I wouldn’t do it again.”
Next week: Using journaling as a tool to minimize the effects of stigma
- Michael P. Levine is Emeritus Professor of Psychology at Kenyon College. He is co-editor of The Wiley Handbook of Eating Disorders (with Linda Smolak, 2015) and of Preventing Eating-Related and Weight-Related Disorders: Collaborative Research, Advocacy, and Policy Change (with Gail L. McVey, Nina Piran, & H. Bruce Ferguson, 2012), and he is co-author of The Prevention of Eating Problems and Eating Disorders: Theory, Research, and Practice (with Linda Smolak, 2006). The 2013 recipient of the Nielsen Award for Lifetime Achievement from the Founders Council of the National Eating Disorders Association, Dr Levine is also a Fellow of the Academy of Eating Disorders, which awarded him their Meehan-Hartley Award for Leadership in Public Awareness and Advocacy in 2006, and their Research-Practice Partnership Award in
References
- Using Writing as a Therapy for Eating Disorders—The Diary Healer is the creative work in my PhD. For details, see https://lifestoriesdiary.com or go to http://acquire.cqu.edu.au:8080/vital/access/manager/Repository/cqu:13833
- Corrigan, P., Larson, J., & Michaels, P. (2015). Coming out proud to erase the stigma of mental illness: Stories and essays of solidarity. Collierville, Tennessee: InstantPublisher.
- Maine, M. D., Samuels, K.L., Tantillo, M. (2015).Eating Disorders in adult women: Biopsychosocial, developmental, and clinical considerations. Advances in Eating Disorders: Theory, Research and Practice, DOI: 10.1080/21662630.2014.999103, 1-11.
 Take part in World Eating Disorders Action Day
Take part in World Eating Disorders Action Day
World Eating Disorders Action Day on June 2, 2018 is a grassroots movement designed for and by people affected by an eating disorder, their families, and the medical and health professionals who support them. Uniting activists across the globe, the aim is to expand global awareness of eating disorders as genetically linked, treatable illnesses that can affect anyone. The Third Annual #WorldEatingDisordersDay will take place on June 2, 2018 with a focus on breaking stigma about Eating Disorders. #WeDoAct2BreakStigma.
Join the virtual campaign on social media and host a local event to share information and advocate for policy change to ensure access to evidence based treatment for all affected.