Traumatic treatment for people with eating disorders must stop

Traumatic treatment for people with eating disorders must stop
Imagine being told: ‘You are naughty and a burden on your family’. Survivor voices are gaining momentum in calling on health professionals to treat their patients with care and respect.
Hospitals are rarely known for their warmth, colour or homely touches; not to be confused with hospitality. They are often characterised by their clinical and cold environments, or their association with pain, tragedy or loss. Therefore, they can be unpleasant or uncomfortable places to be in or visit. Irrespective of how we may differ in our definitions of hospitals, we can agree that they are essential institutions for the provision of care for the injured or sick.
As a young girl, my experience of hospitals was minimal. Aside from being born, I had been fortunate enough not to require a hospital at all. Emerging into adolescence however, I was diagnosed with Anorexia Nervosa. This marked the beginning of numerous hospitalisations and institutionalisations throughout my teenage years and the journey of learning to regain my trust of self, overcoming the fear of relapse and retaking control of my life.
Blaming the person for their illness increases the trauma
Imagine being told as a child struggling with a crippling eating disorder that you are “naughty” and “disobedient” because you refuse to eat. Imagine being told that “you cannot be trusted, that you are manipulative, that you are selfish, that you are vain and that you are a burden on your family and the healthcare system”.
No distinction or attempt at separation is made between yourself as a young girl suffering from a life-threatening and tormenting disease and the disease itself. All the negative and dark thoughts of unworthiness that you are already plagued by from the disease are further reinforced and consolidated by the people and the system that is supposed to help you. Your mind immediately harasses you with this projected perspective; that “you are the problem, that this is all your fault, that you are choosing this and that you can choose to stop your nonsense at any stage”.
Imagine, in addition to this misguided and damaging language, being punished for refusing to eat, taking too long to eat, being caught exercising or using the bathroom without permission. Imagine being scolded or refused basic possessions, privileges or family visitations because of the nature of the disease you are battling; often being denied the very things that could significantly improve your recovery.
The dreadful consequences of punitive care
Fast forward into the future, to a young adult with newly granted control over her life, fearful of making the wrong decision, afraid of it leading to relapse; constantly asking for permission to complete the most menial of tasks (to the annoyance of parents and siblings). “Can I go to the bathroom? Can I have a shower? Can I go for a walk? Can I eat this?” The result of years of enforced dependence on others and the consequences of disobedience. Always questioning; “Am I good enough yet?”.
It is coupled with years of humiliation, the absence of one’s privacy, and the stigma of disdain from those who don’t understand the complexity and internal battle of mental illness. It’s reinforced by a society that paints eating disorders as vain and attention seeking, and it’s perpetuated by a health system still practising punitive treatment.
Let treatment be applied as care, not punishment
Yet, in amongst it all, change in the world is happening, understanding is growing and treatment is improving. The reality is that there will, sadly, always be a place for compulsory treatment of Anorexia Nervosa, as the condition is life-threatening. The truth is that recovery will always require some elements of restriction to an individual’s freedom and choice at times. However, in the mind of a frightened, confused and struggling young girl, these necessary compulsions and restrictions can be experienced as care, rather than punishment through the way the treatment is delivered and the level of relationship developed with those who deliver it.
Survivors are using their voices to challenge stigma, and create change
Here’s to: the survivors of eating disorders that use their voices to challenge stigma and create change, the health professionals who listened to me and my family with empathy not judgement, the doctors that didn’t see me as a problem to solve but a person to love, the nurses that saw “specialling” me not as a waste of their time but as an opportunity to develop relationships, the friends who braved the hospital and the discomfort to bring joy and laughter and my family for their grit, sacrifice and love; for empowering the voice inside of me and never giving up on me even when I’d given up on myself. Finally, my faith has been a constant source of strength and hope for me.
I was that frightened, confused and struggling girl. I required the compulsory and restrictive treatment, I experienced and witnessed firsthand the ‘good, the bad and the ugly’ sides of treatment for those suffering from Anorexia Nervosa. Yet, I was blessed. I had a team on the ground; my parents, railing day and night on my behalf, to keep me alive and to give me a future. Their sacrifice and the subsequent sacrifice of my siblings led me in 2007 to the treatment offered at The Oak House in Melbourne. A beautiful home full of warmth and hospitality; the stark contrast of a hospital.
Family-based care made all the difference
The Oak House was an outpatient centre for treating eating disorders. My mother had come across the clinic in her research of the Maudsley Approach, or family-based treatment, to the treatment of eating disorders. The Maudsley Approach is an intensive outpatient family and evidenced-based treatment where parents play an active and positive role in their child’s recovery; from weight gain and management to releasing the control of food back to the child and encouraging expected adolescent development.
For the first time, my parents were seen as resources to my recovery rather than contributors to my disease and were allowed to share their own experiences and struggles with the illness. The Oak House had a multidisciplinary team of health professionals including dieticians and psychologists; that holistically worked with families and individuals to provide support. I was fortunate enough to attend The Oak House after years of unsuccessful improvement in my condition and in doing so began a new chapter in my recovery; one of feeling understood, heard, empowered and included. Sadly, The Oak House was forced to close its doors in 2010 due to insufficient funding.
Today, I am encouraged to see that more in-patient and out-patient clinics are operating within Australia in similar stead to The Oak House. That there have been changes to treatment delivery for patients with eating disorders in hospitals. However, families and individuals continue to face significant barriers to treatment; including accessibility, affordability, stigma, location and sustainable funding of these programs/clinics.
This is why I hope by sharing with you all, we can continue to bring these issues into the light and as a collective, we can continue to advocate for change, healing and hope for those who follow in our footsteps.
Special note: Kristen’s story, and that of her family, is one of the 10 stories shared in the book, My Kid is Back – Empowering Parents to Beat Anorexia Nervosa, by Daniel Le Grange and June Alexander.
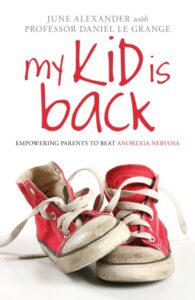
My Kid is Back explains how family-based treatment can greatly reduce the severity of anorexia nervosa in children and adolescents, allowing the person with the illness to return to normal eating patterns, and their families to return to normal family life.
In this book, 10 families share their experiences of living with anorexia. Parents describe their frustrations in seeking help for their child and dealing with their behaviour and sufferers discuss how the illness gets into their mind and takes over their personality.
By focusing on the Maudsley family approach and expert advice from Professor Daniel Le Grange, and including clear lists of illness symptoms, strategies for parents and carers to follow, and information on getting further treatment and support, this book proves a helpful resource for families who want to win the battle with anorexia nervosa.
- My Kid is Back – Empowering Parents to Beat Anorexia Nervosa. June Alexander and Prof. Daniel Le Grange. Routledge (London). 2010.