A reminder that one day the diary that is my life serial will end
I was photographing granddaughters at horse riding, when suddenly I was unconscious on the ground
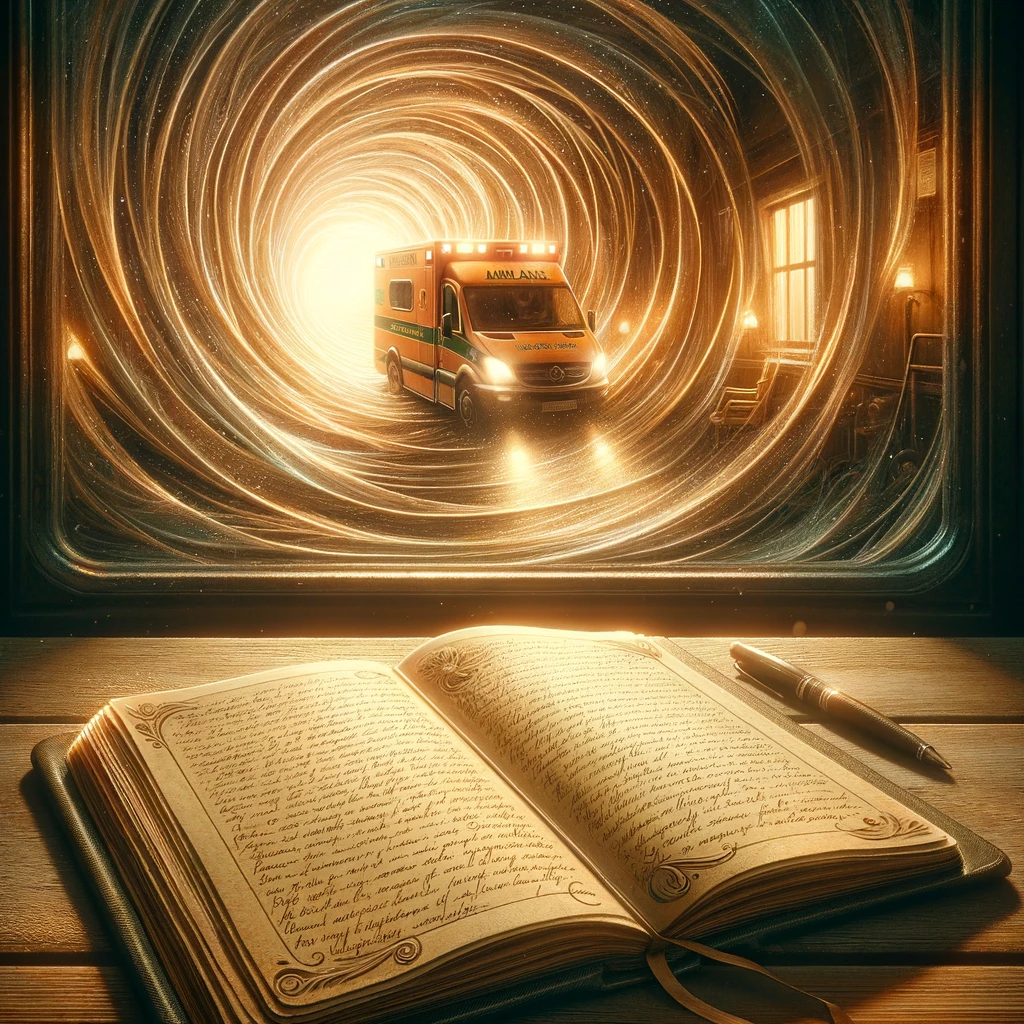
A reminder that one day the diary that is my life serial will end
Yesterday was one of those days that did not work out as planned.
All went well, initially. I was in the local, heated, 50m outdoor pool by 6.10am, doing a half-hour of prescribed exercises. I love being in the water. Then I came home, showered, and took Maisie for a walk on the clifftops. I ate a bowl of cereal for breakfast and at 9am drove 15 minutes to the equestrian centre to watch two granddaughters at their riding lesson. At 10am I planned to be home, to connect to livestream to watch a grandson play in an international tennis tournament semi-final. I figured I would do some client manuscript editing in the afternoon. My wellbeing cup was full to the brim.
I was happily photographing my granddaughters on their ponies as they went over the jumps in the outdoor ring of the equestrian centre. The lesson finished and I was watching the girls lead their ponies back to the stable.
Happy one minute, unconscious the next
The first clue that something was wrong was when my sight became blurry. Within seconds I could not see and felt I was being drawn into a hole like one feels when being anaesthetised for an operation.
I managed to grab the timber railing for support and call to my daughter Amanda, a few metres away, ‘Amanda I can’t see’. I don’t remember anything after that until I came around. I was lying outside the arena on the soft, green freshly mown grass, with glorious sunshine above. Amanda was calling, ‘Breathe, Mum, breathe,’ but I could not respond to her instructions and could not speak.
Then an equestrian staff member made her presence felt on the other side of me and she spoke quite in my face, firmly and compassionately. With Amanda and this woman and another staff woman, all of whom had First Aid training, I began to be able to respond. They had called an ambulance and to me, it seemed only seconds before two paramedics arrived and took control, carrying out tests including an ECG in the ambulance. The paramedics concluded I had a choice: either go to the hospital now with them or see a GP “TODAY”. I looked to my daughter, and we chose the GP.
God was smiling on me (thank you, Lord) because a) I had immediate help from Amanda (visiting from the city for the holidays) and equestrian staff when the incident occurred, followed by the speedy arrival of the paramedics; b) a GP appointment was available within the hour and the GP said she needed to check for brain bleed or mini-stroke. She organised an urgent brain scan; c) this scan was carried out within two hours, again only minutes from home; d) the GP phoned late in the afternoon to confirm, “your brain scan is clear,” (relief); e) more tests have been arranged and another GP appointment organised. I’m full of gratitude for this caring support.
I feel for my daughter who had a shock. I was ‘out to it’ but she was in the moment – she later said she didn’t know for a time if I were dead or alive. This was the first time she had been called upon to apply her First Aid training and in catching me, as I crumpled from the fence, she was amazed at how heavy an unconscious person can be. She followed her training by the book.
Take heed and be prepared
One moment I was soaking up the beautiful early morning sunshine, happy, doing what I wanted to do, and suddenly I was unconscious on the grass.
I figure there must be a lesson to learn from this experience! My four children, who seem much wiser than me, have been forthcoming with advice. My year’s aims have been remapped to include:
- Being proactive and organising support because if I’d been alone when my world went black, I might not be here right now. By catching me, my daughter had saved me from the risk of hitting my head.
- Inquiring about My Aged Care assistance that our Federal Government provides to help seniors stay in their own homes. We are fortunate in Australia to have various avenues of support – we just need to know how to access this support.
- A major concern is my pets. If I am suddenly admitted to the hospital, a plan needs to be in place for emergencies such as this. My pets are my constant companions and help me feel safe and secure. They are part of my family.
- Asking the Aged Care people about acquiring a medical alert alarm, hopefully before my family returns to the city in a couple of weeks. One son suggests an Apple Watch as well.
- Getting my ‘affairs’ in order. Ironically, this incident happened right when I was updating my Will, so that’s in hand.
- I began 2024 aiming to focus on the three ‘Fs’ – Family, Friends and Fun. Purpose is important too. I work part-time (mentoring and editing) and volunteer in the community (life-writing groups, eating disorder advocacy and Rotary). Collaboration with Prof. Daniel Le Grange and Prof. Ivan Eisler, respectively, on books explaining Family Based Treatment and Multi-Family Treatment for eating disorders is also a priority.
- To do all these things, I must be my own best friend and ensure my wellbeing cup is replenished each day.
- Eating three meals and three snacks daily, sleeping sufficiently, and exercising (enough but not too much), are non-negotiables.
The healing power of love
I am grateful to my children for being my cheer squad with this latest little hiccup, and for inspiring me through my greatest battles. They gave me strength when I faced and endured enormous mental health battles over several decades. My children were born to a mother who had a severe eating disorder, chronic anxiety, and depression. They had to grow up with a mother attempting recovery. Together with their dad, who has always been a rock in the turbulence, they all deserve a gold medal. I’m blessed to have their love. The inner turmoil and torment have been long quelled, and I am the most at peace within I’ve ever been.
In many respects, I am continuing to catch up on life, filling the gap the anorexia gnawed in my life over 44 years. However, yesterday’s ‘bombing out’ is a reminder that time is marching on. Every day is precious. No matter how busy the day might be, I always make time to reflect, write and debrief in my diary.
One day the daily serial that is diary-writing will end but words live on
 While lying in the ambulance, my mind was already penning an entry to my diary for the day. I thought, ‘The day will come when my diary ends, and that will be when my life ends.’
While lying in the ambulance, my mind was already penning an entry to my diary for the day. I thought, ‘The day will come when my diary ends, and that will be when my life ends.’
I don’t know when that final entry will come. Until then, every day is a gift, and every day I will continue to write entries in what is now a family diary. Words are my loyal, long-time friends. When something unexpected happens, like collapsing without warning on a perfectly beautiful day, writing helps me to put everything in perspective and move on.
When I’m gone, the words will live on, and this is a comforting thought. I encourage you to keep a diary, too. The benefits are many — for today and tomorrow.





Dr. Alexander, I am so shocked and sorry to hear about your latest health episode as I have had ongoing anorexia since 1972. I am in the process of revising my living will and finding more supportive people to sign up as my POA, ensuring that I have a proper Jewish funeral, and yes, that my “kitty” will be well taken care of. You have been in my thoughts since Thursday’s NYT published an article which made me upset. The article, now part of American NYT’s Magazine is by Katie Engelhart “Letting Naomi Die” who is a 37 year old woman with chronic anorexia under palliative care with Dr. Joel Yager and Dr. Treem at the ACUTE Center for ED. I am hoping that you and other clinicians with respond to the NYT and at ED centers NOT TO ENDORSE PALLIATIVE CARE. People with ALS, renal faiture, etc yes; anorexia no. I struggle, fall, yet rise with the hope and support by you and care givers like Betsy Brenner.
Thank you for your message, Joanna. As someone with long-term anorexia you have more than 50 years of experience to draw on in knowing what is helpful and not helpful in the treatment of this horrendous illness. I strongly believe that there is hope at every age. Improving quality of life one step at a time can lead to the miracle of ‘recovery’. With love, June
I am almost 63. I began my (diagnosed) anorexia life at 12. It’s been 51 years of feeling unworthy, feeling shame, self loathing, having no voice and starving myself. Yes, there have been some better times, my life has been full with 4 children, a teaching career, artwork, etc. Yet the underlying thoughts of sadness, depression, unworthiness, hating my body and mind have endured.
Only recently did I begin my inpt journey. Beginning in 2017, so in my mid 50s, I began that revolving door of treatment, weight restoration, and subsequent relapses inbetween. My aging body has begun to show signs of 51 years of misuse and lack of self care. I’ve had 2 more inpt stays/weight restorations since then, each more miserable than the other.
I am very tired. Not ready to give up the fight, necessarily (but that is today), but I can well understand someone who might be. As someone who also saw beloved family members finally ask, beg for palliative care, why should someone who has endured a similar pain be any different. Is this not once again stigmatizing mental health? Why is the brain any different than any other organ in the body. They become ill. Some can be cured some cannot. It is the pts choice, possibly along with physician clarification, if they wish to continue fighting or to allow nature to take it’s course. With respect, I must disagree with Joanna Katsune. I want the choice to fight or to not fight when I am finally just too tired.
Thank you for sharing your lived experience of a long-term eating disorder – and the effects this has had on your life. I relate to the feelings you describe – our journeys have many parallels. The main difference being that I began ‘recovery’ work in my 30s – a long, long trek of 25 years to get to achieve ’51 per cent healthy self’ and then the journey continued — I empathise with your feelings of tiredness because the struggle to reconnect/rebuild one’s health-self can be relentless – and our body physically reveals and stumbles with the stresses as we grow older – and I agree that the patient’s voice (not their ED voice, although some people with this long term illness explain they cannot discern the difference) needs to be heard and listened to. My experience is that with help, I have achieved peace within, and I wish this for you, too. You deserve it. xo
Hi June 👋
Firstly, Happy New Year. I hope you had a good Christmas and holiday period.
Secondly, it sounds like a bit of a scary/confronting experience that happened for you and your family yesterday – I’m glad that you were able to be seen to quickly outside of the ED and that they were able to rule out a stroke. Have they had any more results that have come through?
First things that come to mind for me as a Paramedic with the symptoms you described are heat stroke/dehydration, stroke, low blood sugar, cardiac arrhythmia… I am glad to hear though that you are doing better and it gave you an opportunity to reflect on some important things to consider in life overall.
I loved how you said “In many respects, I am continuing to catch up on life, filling the gap the anorexia gnawed in my life over 44 years.”. I can relate to this so much, especially since 2021. It’s like my passion and drive have kicked back in and I have become some what addicted (not literally) to challenging myself, growing and stepping out of my comfort zone (a stark difference to the little girl who was fighting for her life for over 15 years) xx
Dear Sally, Thank you for your heartfelt message – I take great joy in following your personal growth on FB, achieving amazing life goals, giving to your community, and being an inspiration for us all. Keeping a life balance requires constant vigilance and we are continually finding out who we are without that dreadful ED voice bossing us around and making us self-doubt. Take care of yourself as well as your patients. I admire paramedics so much — they have been of great assistance to me at crucial moments along my life path. I am continuing to have tests and will provide an update when an outcome is found. I am feeling really good today:-) Love from June
Dear June, I was shocked to read of your own recent health shock. I had a bit of a shock myself recently and found myself in hospital having a TAVI (transcatheter aortic valve implantation) procedure on the 30th of November in Melbourne. I was in complete denial that anything was wrong with me as I had been waiting over four months to see a cardiologist. Everyone always tells me how well I look even though I suffered from a little breathlessness. I had just had cataract surgery with excellent results. While I was in Melbourne I was suddenly referred to a cardiologist surgeon and wondered what all the urgency was about as I felt so well. I have a heart murmur which I didn’t think anything to worry about but had a plaque build-up in my aortic artery which required urgent attention, After a dental check-up up I was in hospital. I was told they got me early before I got worse as it was possible I would have a stroke or heart attack if I didn’t have this procedure. Thank goodness I didn’t have to have open heart surgery as my older sister and brother had had many years before. The procedure I had went up through arteries from my groin. I was awake and didn’t feel a thing and could watch the whole procedure. My recovery was good, I am to have a check-up again soon. I urge everyone to check up on their heart health as heart disease is a silent killer. I love writing and have been doing so all my life about life experiences and farm life. Cheers Ngaere
Dear Ngaere, Wow thank you for sharing your amazing medical emergency experience. I am delighted the procedure went well for you. I hope your check-up reveals all is in fine running order so that you can continue to engage fully in your love of writing. You have many stories to tell about life on the land! June xo